Your next step to smarter billing. Schedule a demo to automate status checks.
Experience hands-free follow-ups, real-time insights, and secure integration - all in one intelligent platform. Let automation do the heavy lifting.
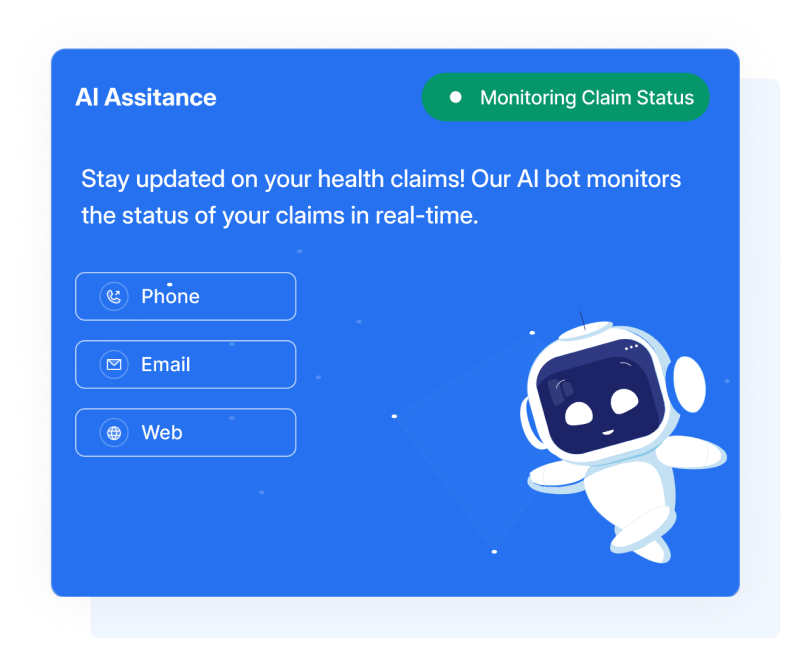
Book a DemoAgentic AI eliminates hours of manual payer outreach — using voice, email, and web automation to check claim statuses in real time.

Built to streamline operational workflows for modern billing teams across all specialties.
From payer calls to portal logins, Agentic AI handles every step of your claim status checks — so your team can focus on what truly matters.
 Voice Automation
Voice Automation
 Email Follow-ups
Email Follow-ups
 Portal Access
Portal Access
 Result Routing
Result Routing
 Payer Coverage
Payer Coverage
 Audit Ready
Audit Ready
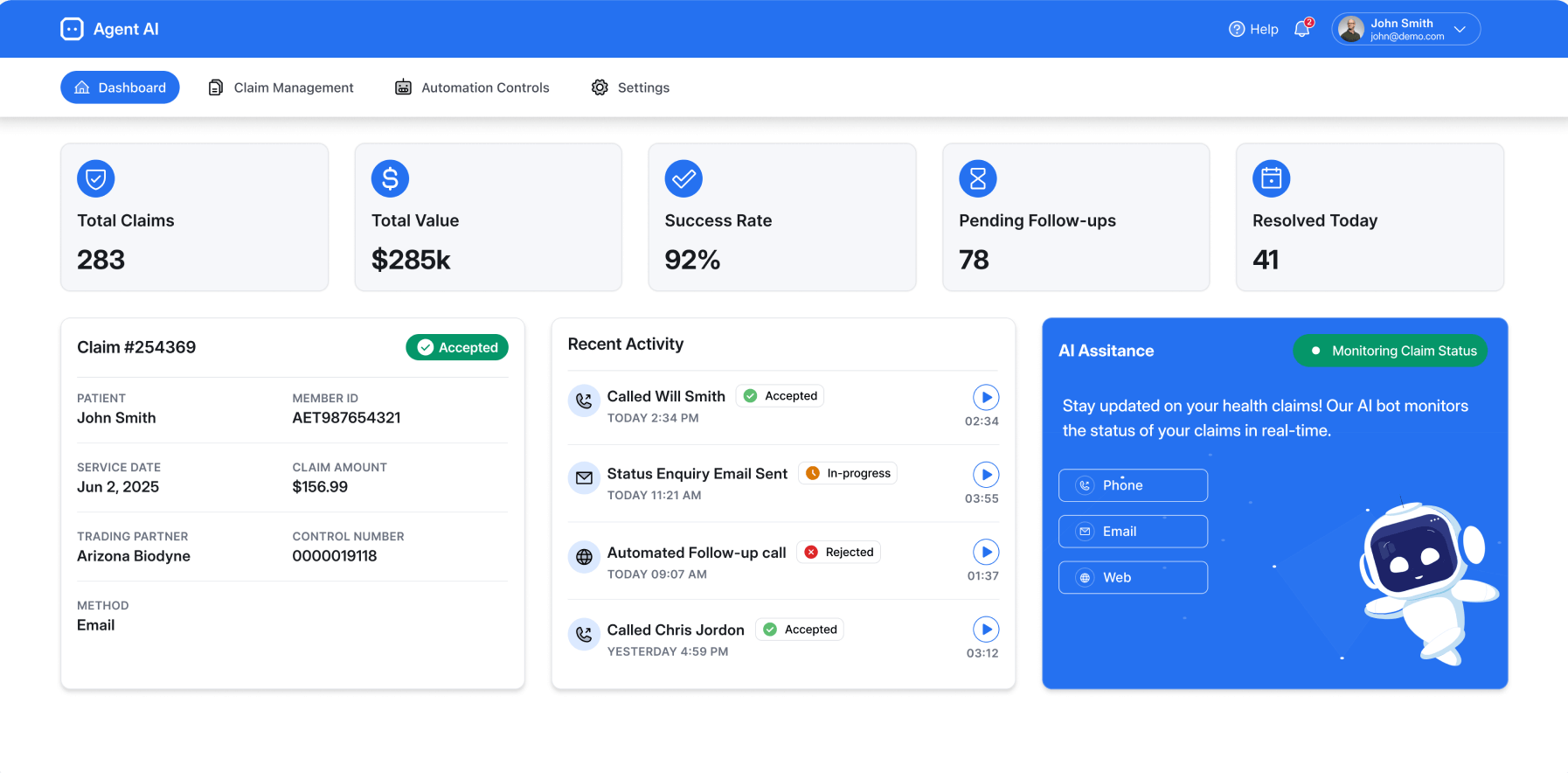
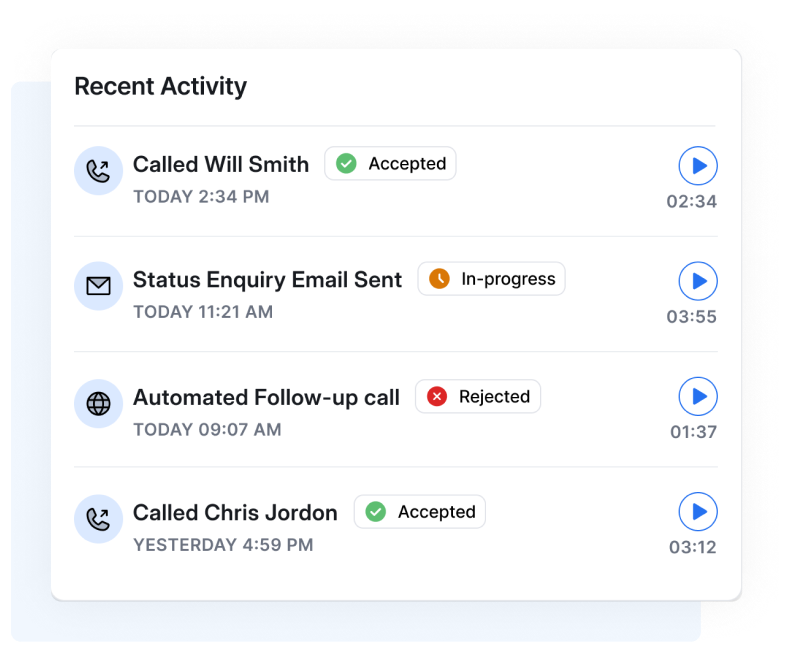
With Agentic AI, your team gets instant visibility into where every claim stands - across all channels - without chasing updates manually.
 Unified Dashboard
Unified Dashboard
 Channel Tracking
Channel Tracking
 Smart Alerts
Smart Alerts
 Secure Recordings
Secure Recordings
 Auto Logging
Auto Logging
 Daily Transparency
Daily Transparency
How automation handles every follow-up — so you don't have to.
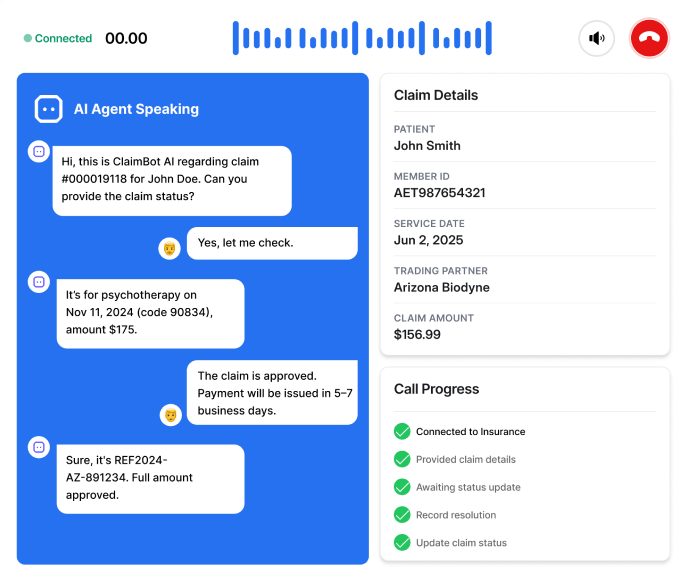
Agentic AI blends voice, email, and RPA automation to manage claim status checks from start to finish. No more manual calls, logins, or spreadsheets — just results delivered directly to your team.

Calls payers, navigates IVRs, and records responses — all without human input.

Sends follow-up emails to payer reps and captures replies automatically.

Logs into payer websites, searches for claims, and fetches real-time updates.

Transcribes results, classifies them, and routes insights to your billing software.

Works in parallel, handling hundreds of claims per day — no added headcount.

Tracks claim statuses and channel performance in real time across voice, email, and portals.
Agentic AI connects with your EHR, RCM, or billing software — no workflow changes, no disruptions. Just smooth automation that fits right in.
Learn More




Automation that delivers real, measurable impact - from day one and beyond.
Agentic AI helps medical billing teams streamline operations, reduce overhead, and improve revenue cycle performance without disrupting existing workflows. Whether you're handling hundreds or thousands of claims, the benefits scale with you.

Processes hundreds of claims daily to help reduce bottlenecks and eliminate delays.

Flags stalled or urgent claims so your team can act faster and smarter.

Reduces A/R days and improves first-pass resolution rates across payers.

Frees staff from repetitive follow-ups so they can handle more complex cases.

Delivers audit-ready logs, call recordings, and a clear trail of every action.

See operational improvements in speed, accuracy, and cost-efficiency from the start.
Agentic AI keeps your billing team aligned with real-time updates on every claim's progress - across voice, email, and portal channels.
Designed for regulated industries that demand privacy, protection, and performance.
 ZeroTrust Architecture
ZeroTrust Architecture
 Multi-Factor Authentication
Multi-Factor Authentication
 24/7 Monitoring
24/7 Monitoring
 CIS-Level 1 Infrastructure
CIS-Level 1 Infrastructure
 Audit-Ready Automation
Audit-Ready Automation
 Regulatory Compliance
Regulatory Compliance
Whether you're an individual, a small team, or a growing enterprise, we have a plan that aligns perfectly with your goals.
Experience hands-free follow-ups, real-time insights, and secure integration - all in one intelligent platform. Let automation do the heavy lifting.
Book a Demo